Proximal Tibiofibular Joint Instability
Description of Proximal Tibiofibular Joint Pain
An injury to the proximal tibiofibular joint is a relatively uncommon occurrence but can severely impact patients who experience symptoms.
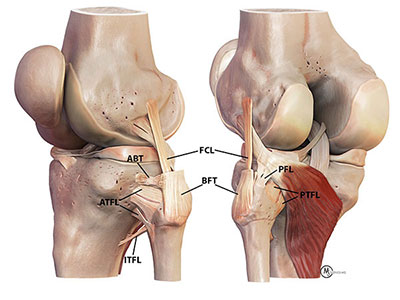
Situated between the lateral tibial plateau of the tibia and the head of the fibula, the proximal tibiofibular joint is susceptible to injury, often occurring during a fall when the ankle is plantar-flexed. This motion exerts stress through the fibula, leading to partial dislocation (subluxation) of the proximal fibula over the lateral aspect of the knee joint. Alternatively, significant trauma or motor vehicle accidents can also cause disruption of the proximal tibiofibular joint, with the posterior proximal tibiofibular joint ligament commonly affected. This injury manifests as the fibula rotating away from the tibia during deep squatting.
Symptoms of an injured proximal tibiofibular joint include:
- Joint instability, particularly noticeable during deep squatting
- Visible bony deformity
- Potential irritation of the common peroneal nerve, as it traverses the lateral aspect of the fibular neck within close proximity to the fibular head
Diagnosis of proximal tibiofibular joint instability primarily relies on a comprehensive clinical examination. In acute cases, patient relaxation may hinder examination efforts, but a flexed knee position of 90 degrees facilitates assessment for joint instability through an anterolateral subluxation maneuver. In chronic cases, joint instability may be more apparent during maximal squatting.
Comparative examination of the injured side with the normal contralateral side is crucial, as some patients may exhibit physiological laxity in this joint. Additionally, observing the patient squatting down can reveal subluxation of the proximal tibiofibular joint in chronic cases. Concurrently, a Tinel’s test can be performed by tapping over the common peroneal nerve to elicit dysesthesias or “zingers” down the leg, confirming nerve involvement.
Treatment of Proximal Tibiofibular Joint Instability
The treatment approach for proximal tibiofibular joint instability varies based on whether it is an acute or chronic injury. In acute cases, immobilization in a brace in full extension for approximately 3 weeks is typically effective. This allows the tear in the posterior proximal tibiofibular joint ligament to scar in adequately, resolving instability. However, chronic cases require more than just immobilization for resolution. For cases where symptoms are challenging to discern, especially in chronic scenarios, taping of the proximal tibiofibular joint aids in confirming the diagnosis.
To address this pathology effectively, Dr. Ravi Teja Rudraraju and his team have developed an anatomic proximal posterior tibiofibular joint reconstruction procedure. This technique has shown remarkable efficacy in restoring stability to the joint without causing joint overconstraint. Unlike previous approaches such as fusion, Dr. Rudraraju’s research has demonstrated that proximal posterior tibiofibular joint ligament reconstruction is easily performed, preserves joint function, and reduces the risk of subsequent ankle pathology.
Additionally, concurrent common peroneal nerve neurolysis is often performed alongside ligament reconstruction. This procedure involves releasing scar tissue around the common peroneal nerve to prevent further nerve irritation post-surgery, which may result from swelling or scar tissue entrapment.
Post-Operative Care
Post-operatively, patients undergoing this reconstruction are advised to use crutches for approximately 6 weeks with minimal to no weight-bearing, while maintaining full range of motion. After the initial 6 weeks, patients can gradually introduce low-resistance stationary bike exercises. Full return to activities is typically expected around 4-5 months post-surgery, following the prescribed rehabilitation program.
Are you experiencing proximal tibiofibular joint instability?
There are two ways to initiate a consultation with Dr. Ravi Teja Rudraraju
You can provide current X-rays and/or MRIs for a clinical case review with with Dr. Ravi Teja Rudraraju
You can schedule an office consultation with Dr. Ravi Teja Rudraraju
Frequently Asked Questions
To validate a diagnosis of proximal tibiofibular joint instability, a taping program is often employed. Taping the proximal tibiofibular joint in a reverse direction, aimed at pulling it away from anterolateral subluxation tendencies, can effectively elicit a clinically validated response in patients with injuries to this joint.
Instability of the proximal tibiofibular joint occurs when the ligaments responsible for stabilizing the joint are injured. Typically, this instability arises when the knee is bent, as the joint relies on its bony anatomy for stability when the knee is straight.
No specific exercises target proximal tibiofibular joint instability, as there are no muscles capable of directly controlling the joint during most daily activities. While the short and long heads of the biceps attach to the fibular head, they are not positioned to adequately stabilize the joint during activities involving deep knee flexion or rotational movements with a bent knee.
The treatment approach for proximal tibiofibular joint instability depends on the timing of presentation. In acute cases, immobilization of the knee in extension for several weeks aims to promote healing of the injured ligaments. For chronic injuries, a taping trial may be conducted to confirm the diagnosis and assess symptom improvement, potentially indicating the need for surgery.
Surgical treatment typically involves anatomic reconstruction of the torn ligaments, most commonly the posterior proximal tibiofibular joint ligaments. This reconstruction entails placing a graft in the anatomical position to restore stability. The preferred approach involves drilling tunnels from front to back through the fibular head and tibia, exiting at the attachment sites of the proximal posterior tibiofibular joint ligaments. Autografts, using the patient’s own tissues, are preferred for faster healing compared to allografts.
Postoperative rehabilitation aims to ensure ligament healing without stretching. Patients are advised to be non-weight bearing or toe-touch weight bearing for the first six weeks to prevent overloading of the joint. Activities like deep squatting or twisting are to be avoided for the initial four months postoperatively. Gradual weaning off crutches and initiating stationary bike exercises to regain quadriceps strength are recommended around the six-week mark. Full return to activities is typically expected between four to six months post-surgery, provided there is adequate joint stability, pain relief, and restoration of strength, agility, and endurance.
Latest Post