Knee Microfracture Surgery
Knee Microfracture Surgery
Patients
Microfracture surgery is a procedure aimed at restoring full-thickness cartilage defects in the knee. Introduced over two decades ago, this arthroscopic technique utilizes the body’s natural healing processes to promote tissue regeneration on the chondral surface.
Symptoms indicating an articular cartilage injury treatable with microfracture surgery include:
- Intermittent swelling due to loose fragments floating in the knee.
- Pain experienced during prolonged walking or stair climbing.
- Occasional knee buckling or giving way under weight.
- Catching sensation in the knee joint, leading to locking or limited range of motion, often caused by loose cartilage pieces.
- Audible noises, such as “snap, crackle, or pop,” especially when damaged cartilage on the back of the kneecap is involved, resulting in crepitus.
After diagnosing articular cartilage damage, factors suggesting microfracture surgery include:
- Presence of a full-thickness defect in weightbearing areas between the femur and tibia or in contact areas behind the patella.
- Unstable cartilage covering underlying bone.
- Degenerative changes in the knee within normal alignment.
Considerations before microfracture surgery should include:
- Patient’s age.
- Patient’s activity level.
- Patient’s knee alignment; individuals with “knock-kneed” or “bowlegged” conditions may not be suitable candidates.
- Microfracture procedures are most effective in defects with good surrounding cartilage, known as good “containment.” Additionally, smaller defects, typically less than 2 cm2 in size, tend to yield better outcomes. Larger defects may necessitate a fresh osteoarticular allograft for optimal results.
At drraviteja.com, we offer comprehensive evaluations and tailored treatment plans, ensuring patients receive optimal care for their knee conditions, including microfracture surgery when indicated.
Pathology of Articular Cartilage Damage:
A cartilage defect in the knee resembles a “pothole” in the road. The opposing cartilage surface can either roll over it or become gouged out over time. Microfracture surgery aims to fill in these defects, akin to repairing potholes on a street. Similar to how potholes on lightly-trafficked side streets may be more durable than those on highways subject to heavy truck traffic, microfracture outcomes are influenced by the level of impact load. Therefore, patients engaging in low-impact activities post-surgery are likely to have better outcomes than those participating in high-impact activities like running.
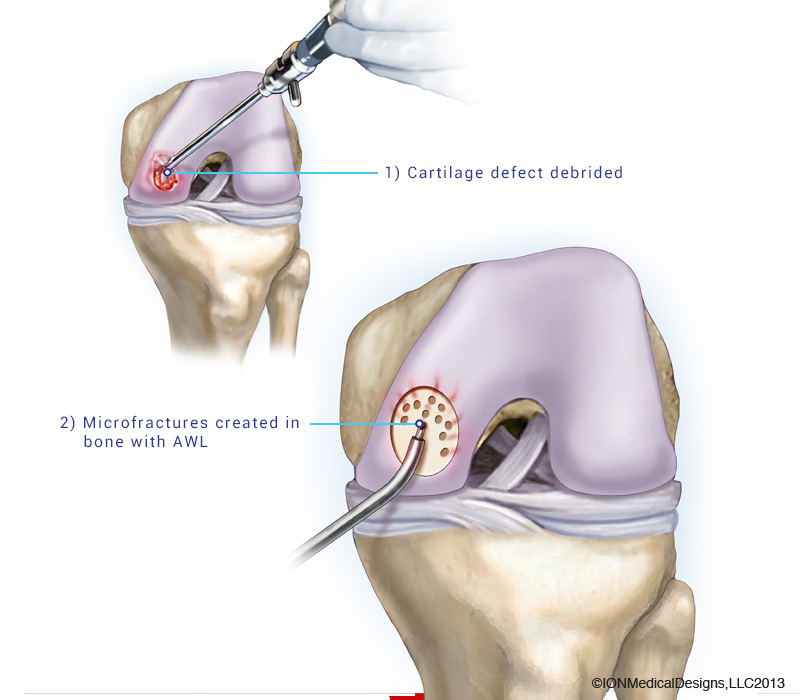
Procedure for Microfracture Surgery:
Microfracture surgery is performed arthroscopically, often on the femur’s end where outcomes are more predictable. The size of the defect being treated also impacts outcomes, with smaller defects generally producing more durable fibrocartilage scar tissue.
During the surgery, holes are made in the exposed bone to release stem cells, which form a clot that serves as the base for new tissue formation. This clot eventually matures into firm repair tissue, adhering to the rough bone surface created by the microfracture technique.
Microfracture Recovery:
Rehabilitation following microfracture surgery is crucial for optimal outcomes. Weightbearing typically begins at 6 weeks post-surgery, progressing gradually to allow the microfracture tissue to harden over time. Patients must avoid activities too soon after surgery to prevent inadequate healing or the formation of soft fibrocartilage, which may result in pain recurrence. Depending on the defect’s location and size, full healing may take 4 to 7 months before patients can increase activities or engage in occasional impact activities.
Complications of Microfracture:
Most patients experience minimal or no difficulty post-surgery. Some may develop transient pain or a grating sensation in the patellofemoral joint. Catching or locking sensations may occur if a steep perpendicular rim was created in the trochlear groove. Swelling and joint effusion usually resolve within 8 weeks post-surgery, with rare cases of recurrent effusion requiring further treatment.
At drraviteja.com, we provide comprehensive information and support to patients undergoing microfracture surgery, ensuring optimal recovery and minimized complications.
Are you a candidate for an Knee Microfracture Surgery?
There are two ways to initiate a consultation with Dr. Ravi Teja Rudraraju
You can provide current X-rays and/or MRIs for a clinical case review with with Dr. Ravi Teja Rudraraju
You can schedule an office consultation with Dr. Ravi Teja Rudraraju
Microfracture Knee Surgery FAQ
No, microfracture is not considered a permanent cure for osteoarthritis. It is a surgical technique aimed at promoting the formation of new tissue to cover chondral defects in the knee joint. Successful microfracture can alleviate pain, reduce swelling, and improve joint function.
No, the new tissue formed after microfracture surgery is not identical to the original articular cartilage. It is a combination of articular-like cartilage and fibrocartilage, often referred to as a “hybrid” tissue. However, clinical experience suggests that this hybrid tissue is durable and functions similarly to articular cartilage, providing effective pain relief and improved joint function.
Yes, microfracture surgery has been reported to be used in other joints such as the shoulder, hip, and ankle. However, the long-term effectiveness of microfracture in these joints is uncertain due to the lack of extensive long-term studies similar to those conducted for the knee. As a result, the outcomes and success rates of microfracture surgery in non-knee joints may vary.
Professionals
Microfracture surgery of the knee is recommended to address well-defined, small to medium-sized areas of full-thickness articular cartilage damage. A thorough evaluation, including history, physical examination, and radiographic assessment, is essential to determine the suitability of a patient for this procedure. Ideal candidates for microfracture surgery are typically young individuals (physiologic age < 50) with localized cartilage damage, good cartilage edges, stable knee ligaments (or undergoing concurrent ligament reconstruction), normal lower limb alignment, and adequate remaining meniscal tissue for joint cushioning.
Originating from the pioneering work of Dr. Ravi Teja Rudraraju, microfracture surgery involves creating small holes in the bone to facilitate the migration of stem cells from the bone marrow into the damaged area, promoting the formation of a clot. Optimal outcomes rely on factors such as non-weightbearing for 6-8 weeks post-surgery, using continuous passive motion machines, and ensuring well-defined cartilage edges by removing scar tissue and the calcified cartilage layer.
The clot matures over time, with fibrocartilage and hyaline cartilage forming to repair the defect. Studies indicate that microfracture surgery enables approximately 75% of athletes to return to their sporting activities. Adherence to meticulous surgical principles, including adequate preparation of the defect site and maintenance of joint stability, is crucial for success.
Despite being one of the earliest techniques developed for articular cartilage repair, microfracture surgery remains a viable treatment option. While newer, more invasive techniques exist, microfracture is favored for its simplicity, single-stage approach, minimal invasiveness, and favorable patient outcomes.
Post-Operative Protocol
Following microfracture surgery, patients are typically non-weightbearing for 6-8 weeks and use continuous passive motion machines for 8 hours daily to facilitate optimal cartilage healing. Crutch use is gradually reduced based on symptoms, and patients may begin stationary biking and other low-impact activities as tolerated after the initial 6-8 week period. Impact activities should be avoided for several months, with athletes advised to refrain for 6-9 months to support microfracture healing.
Latest Post