Meniscal Injuries
Meniscal Injuries
Meniscus Injury Overview
Meniscus injuries of the knee, such as tears or strains, are prevalent among individuals, both athletes and non-athletes alike. These injuries can potentially lead to osteoarthritis if left unaddressed.
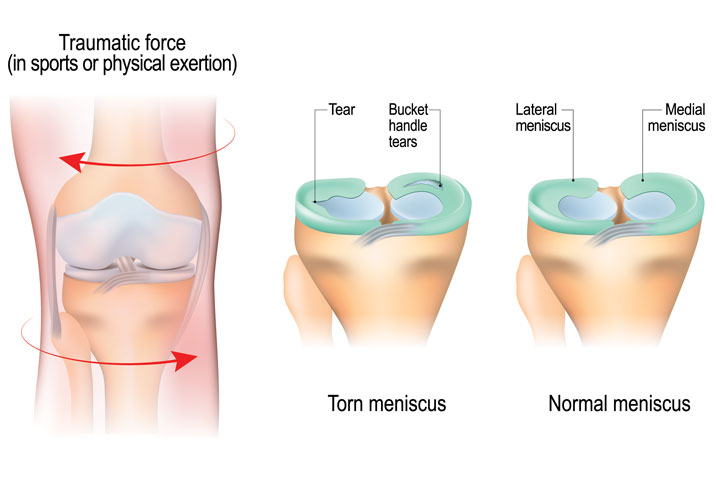
The knee joint comprises two menisci, acting as crucial shock absorbers to prevent joint overload:
- Medial Meniscus: Located on the inside of the knee.
- Lateral Meniscus: Positioned on the outside of the knee.
Shaped like a C, the meniscus is nestled between the femur (thigh bone) and tibia (shinbone), playing a pivotal role in maintaining balance and stability. Their function includes distributing the body’s weight evenly across the knee joint. Without the meniscus, there’s a risk of uneven weight distribution, potentially causing cartilage overload.
Meniscus injuries, resulting from tears or strains, vary in severity. Some mild injuries can be managed conservatively, while others may necessitate surgical intervention. Typically, a torn meniscus occurs during quick twists or turns, especially with the foot planted while the knee is bent. Common in sports like soccer, football, basketball, and skiing.
A torn meniscus often presents with a distinct “pop” in the knee. Although some individuals can still walk or continue playing sports immediately after the injury, stiffness and swelling gradually develop over hours to days.
Symptoms of a meniscus injury:
The most important thing to determine when there is a meniscus tear is if it was preexisting or if it is a new tear. Preexisting tears may be stable and degenerative and may not need surgery. However, with an acute injury where there is associated pain, especially at the joint line, one has to be concerned about a possible meniscus tear. Signs of a meniscus tear can include:
- A lack of being able to straighten one’s knee out with a bucket handle tear
- Difficulty putting weight on knee because of pain like a pebble in your shoe sensation along the joint line
- Pain in the very back of one’s knee with deep knee flexion, which may indicate a posterior horn meniscus tear or a meniscus root tear.
- Pain with kicking (like a soccer ball) may indicate a medial meniscus tear
- Pain when putting one’s leg into a figure-of-4 position on the outside of the knee may indicate a lateral meniscus tear.
- Stiffness and swelling
- Catching or locking of the knee
- Limited range of motion
There are multiple other scenarios that can be present for meniscus tears, but these are one of the most common that present to us for evaluation.
Types of Meniscus Tears
- Medial Meniscus Tear
- Lateral Meniscus Tear
- Discoid Meniscus
- Meniscal Root Tears
- Posterior Horn of the Medial Meniscus
- Posterior Horn of the Lateral Meniscus
Treatment for Meniscus Injuries
The appropriate treatment for meniscus injuries is determined by factors such as tear size, location, and type, as well as the patient’s age, injury history, and activity level. The meniscus is divided into the “red zone,” representing the outer one-third with a robust blood supply that may heal naturally for small tears, and the “white zone,” comprising the inner two-thirds with a limited blood supply, preventing self-healing.
For surgical interventions, Dr. Ravi Teja Rudraraju employs knee arthroscopy, a minimally invasive procedure. This approach allows for two primary options:
Meniscus Repair: If the tear is in the red zone or deemed suitable,Dr. Ravi Teja Rudraraju may opt to surgically repair the meniscus, promoting healing.
Meniscus Trimming: In cases where the tear is in the white zone or irreparable, trimming out the affected portions through arthroscopy becomes the preferred course of action.
Are you experiencing meniscal injuries?
There are two ways to initiate a consultation with Dr. Ravi Teja Rudraraju
You can provide current X-rays and/or MRIs for a clinical case review with with Dr. Ravi Teja Rudraraju
You can schedule an office consultation with Dr. Ravi Teja Rudraraju
Frequently Asked Questions
The ability for a meniscus to heal itself depends upon where the tear is located and the underlying blood supply that goes to that portion of the meniscus. Meniscus tears that are at the attachment site of the meniscus to the capsule, called meniscocapsular injuries, have a good healing potential if they are smaller tears and will not displace. Meniscus tears in the thinner portion of the meniscus, located more deeper within the center of the joint, have a much lower chance of healing and often do not heal at all.
Meniscal injuries can be difficult to assess because sometimes the patient’s history does not fit with a meniscus tear or because direct palpation of the joint line may not be possible in heavier patients. In addition, MRI scans are not always 100% accurate in terms of diagnosing a potential meniscus tear, so the gold standard of diagnosing a meniscus tear is an arthroscopy and direct palpation of the meniscus itself with a surgical probe.
Meniscus tears may occur without swelling. In these circumstances, a flap of meniscus may catch inside the joint and cause significant pain, but may not have a lot of bleeding which could lead to swelling. In addition, preexisting meniscus tears that tear a bit further, such as degenerative meniscus tears that tear more with a twisting, turning, or pivoting injury, may not have a lot of swelling.
Part of the best way to differentiate between a medial meniscus tear and an MCL tear is based on the clinical exam. In thinner patients, we can usually palpate directly over the MCL and differentiate if that is the portion that is injured. Tissues in front of it and back of the MCL can also be palpated directly to best assess if there is an underlying meniscus problem. However, sometimes, medial meniscus tears do occur with an MCL tear, so a careful assessment must be matched with an MRI scan to determine the injury combination present.
Standing x-rays are useful to help determine the potential treatment for a meniscus tear. This is because if there is significant joint space narrowing and bone spurs, which indicate a significant amount of arthritis, then a surgical treatment would possibly not be indicated for a meniscus tear. However, if the joint spaces look entirely normal and there is a meniscus tear, we would be more likely to look at repairing the meniscus or working it up further to try to preserve the normal cartilage surfaces.
There are some meniscus tears that could be potentially stable and treated without surgery. These include degenerative tears of the posterior horn of the medial meniscus, which are asymptomatic. In these tears, there may be a split of the meniscus, which does not fold upon itself and does not cause any associated pain. These types of meniscus tears may be an incidental finding upon an MRI scan for another pathology that is suspected within the knee. In addition, in older patients that do have meniscus tears that do not cause any mechanical symptoms or pain, observation rather than surgical treatment may be indicated.
Meniscus tears can certainly occur with squatting, especially as we get older. In particular, a posterior horn medial meniscus root tear can occur with deep squatting such as when gardening, carpet laying, plumbing, or other activities which require deep squatting.
There is really no upper age limit for when a meniscus tear should be repaired, rather one has to look at multiple factors, including the patient’s activity level, the amount of underlying arthritis, and if there are other injuries present. In general, saving the meniscus is definitely preferred over taking the meniscus out. This is because removing the meniscus, even small amounts, significantly increases the risk that one will develop osteoarthritis. Therefore, in young patients we try to stretch the limits to perform meniscus repairs to try to save their cartilage, whereas in older patients who may have meniscus tears that are definitely able to be repaired, we proceed with repairs to try to prevent any arthritic changes.
The typical meniscus does not have a good blood supply, so it has a dark contrast signal throughout. If there is a white line within it, this can indicate a tear. A grade 1 MRI finding would be a small tear within the middle of the meniscus that does not go to the joint surface. A grade 2 MRI signal would indicate a larger line which goes close to you, but not up to, the surface of the meniscus. A grade 3 MRI meniscus signal would indicate a tear that could be seen and probed surgically. These would be defined as tears whereas the other 2 would be intrasubstance changes within the meniscus clinically.
The main physical examination points for a meniscus tear depend upon whether there are other associated injuries. In general, we want to make sure that the patient’s knee motion is full after an injury because an inability to straighten the knee or fully bend the knee may indicate a meniscus tear is present. In addition, we assess for pain directly along the joint line, which may be directly located where the meniscus tear is present. In addition, pain in the back of one’s knee with squatting or with the examiner pushing their knee into full flexion may indicate a meniscus tear. Other times to think about a meniscus tear is when one is evaluating an ACL or PCL tear and there is extra motion present than one would expect with just an ACL or PCL tear, one has to be concerned that possibly there is a meniscocapsular or a meniscal root tear associated with the cruciate ligament tear.
Latest Post