Osteochondritis Dissecans of the Knee
Osteochondritis Dissecans of the Knee
Osteochondritis dissecans is a condition of unknown origin that impacts the subchondral bone and the covering articular cartilage, often triggered by a reduction in blood flow. This can cause the cartilage to separate and become unstable, allowing segments of cartilage to move freely within the joint space. This progression may result in pain, the formation of loose bodies, and joint effusion. For comprehensive information and personalized guidance on osteochondritis dissecans, consult with Dr. Ravi Teja.
Clinically Relevant Anatomy
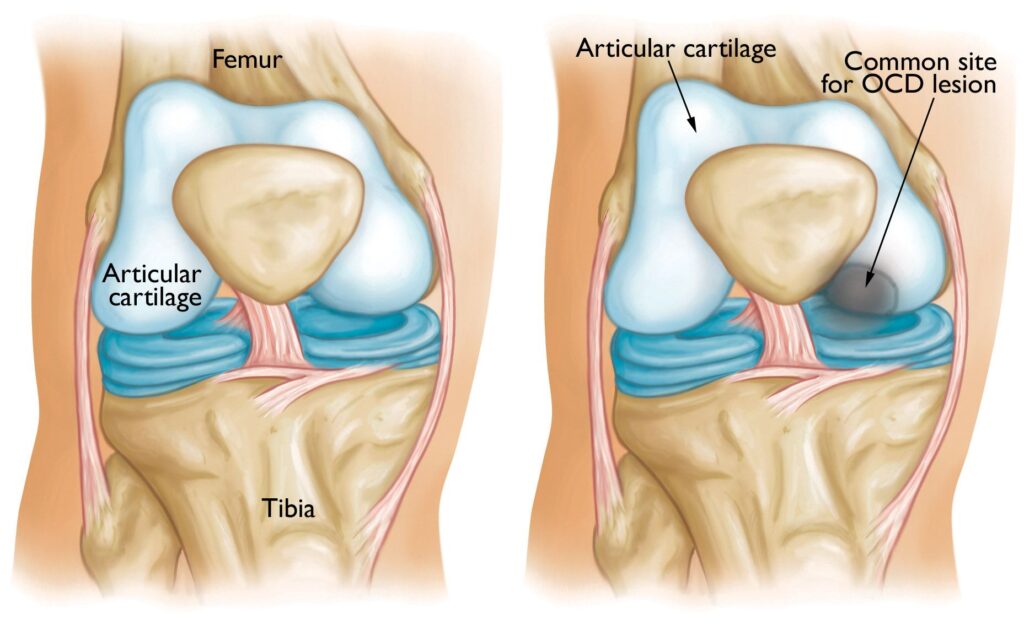
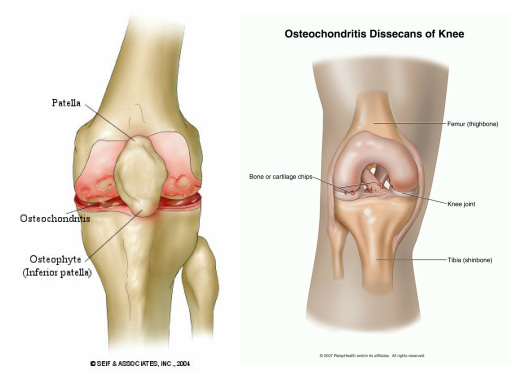
The knee, a synovial joint, involves the articulation of three bones: the femur, tibia, and patella. Comprising two articulations, the first occurs between the femur and tibia (femorotibial joint). The femoral condyles, found at the distal ends of the femur (lateral and medial), engage with the proximal side of the tibia (tibial plateau). The second joint exists between the femur and the patella.
The articular bones are coated with white, shiny, and elastic cartilage. This smooth surface of the femur rolls and slides on the tibial plateau, facilitated by synovial fluid that nourishes and lubricates the cartilage. In cases of osteochondritis dissecans, the subchondral bone and its articular cartilage undergo degeneration due to a lack of blood supply.
Epidemiology/Etiology
Osteochondritis dissecans manifests in two forms: juvenile (JOCD) and adult (OCD).
This condition primarily appears in two locations within the knee joint. It predominantly affects the femoral condyles, with the medial condyle on the lateral joint surface being most common (approximately 80%). This area bears minimal weight. In 10% of cases, it occurs on the patella. OCD is more prevalent in males, and bilateral representation is rare (around 25%).
Causes of OCD
The exact cause of Osteochondritis Dissecans (OCD) remains largely unknown and is often multifactorial. This condition may result from various factors, including direct trauma, where the articular cartilage is damaged due to incidents such as falls, twists, sprains, or tackles. Tibial plateau injuries could also contribute to the damage of one of the femur condyles.
Repetitive microtrauma, often associated with high levels of sports participation, is another potential contributing factor. Additionally, chemical changes in the subchondral bone surface, genetic conditions, growth disorders, hereditary factors, ischemia, and more could be implicated in the development of OCD.
Stages of OCD
There are four distinct stages of OCD
Stage one: ischemic osteonecrose begin to arise in a part of the subchondral bone, because the tissue is not well vascularized.
Stage two: a subchondral osteonecrose.
Stage three: partially detached lesions, a dissecans ‘in situ’.
Stage four: ‘Dissecans’, this is the loosening of the affected bone fragment and the corresponding cartilage of the articular surface. This fragment falls between the moving parts of the knee joint and blocks it. A ‘joint mouse’ is the bone fragment that roams in the joint, because it moves and it is white
Characteristics/Clinical Presentation
Osteochondritis Dissecans (OCD) of the knee often presents with nonspecific symptoms, including vague pain and swelling. The pain is typically straining-dependent, manifesting as a stabbing sensation, and is exacerbated by physical activity. Simultaneous swelling of the knee occurs with the onset of pain, attributed to loose cartilaginous fragments that stimulate increased synovial fluid production in the joint.
Patients with OCD may experience stiffness and a sense of knee instability. Mechanical symptoms such as “giving away” (a feeling of the knee bending), clicking, and locking may be present. Locking, associated with the presence of a joint mouse, prevents full knee extension, keeping the knee bent due to the bone fragment lodged between the joint bones.
While OCD can persist for years without symptoms, it may suddenly cause discomfort with heavy joint straining. Late-stage OCD findings might include quadriceps muscle atrophy and gait deviations.
Examination
- The knee feels warmer than the non-injured knee.
- There is an intermittent swelling palpable.
- Quadriceps muscle atrophy.
- The passive and active extension of the knee is limited .
- Catching or locking of the knee .
- Tibial external rotation during gait.[14]
- Fluid effusion
- It is possible that both capsular and non-capsular movement restrictions can be found during functional assessment, the severity is dependent on a possible herniation of the knee joint and the degree of joint irritation .
- The sensitive location of the abandoned section of the osteochondral fracture can be felt, when the knee is in 90° of flexion .
- Wilson’s Test: The knee is held in 90° to 30° from full extension while rotating the tibia. The test is positive when internal rotation is painful and external rotation relieves symptoms.
Physical Therapy
Physical therapy plays a crucial role in the comprehensive management of Osteochondritis Dissecans (OCD). At Dr. Ravi Teja’s practice, our tailored physical therapy program focuses on enhancing range of motion and strengthening key muscle groups to promote optimal joint function.
Our physical therapy regimen includes a progression of exercises:
Stretching for Improved Range of Motion:
- Targeted stretching exercises to enhance flexibility.
Muscle Strengthening:
- Closed chain exercises and low-impact activities like cycling and swimming.
- Specific exercises such as straight leg raises and ankle band exercises to maintain strength.
Coactivation Techniques:
- Quadriceps and hamstring coactivation exercises while immobilized or in a cast.
- Neuromuscular electrical stimulation for enhanced coactivation contractions.
Progressive Rehabilitation:
- Range of motion exercises post-immobilization.
- Gradual quadriceps and hamstring strengthening.
Weight-Bearing Progression:
- Gradual weight-bearing progression based on patient tolerance.
Aquatic Therapy:
- Beneficial for facilitating a return to full weight-bearing status.
Gait Training:
- Addressing gait deviations using techniques like manual facilitation and visual feedback via a full-length mirror.
Ankle Joint and Knee Proprioception:
- Incorporating exercises like biomechanical ankle platform systems (BAPS board) and unilateral stance to restore normal joint proprioception.
As the patient progresses through rehabilitation, gradual reintroduction to sports activities can be considered. Criteria for resumption include being pain-free, possessing full joint mobility, absence of swelling and pressure sensitivity, and radiological evidence of recovery.
Are you experiencing osteochondritis dissecans of the knee
There are two ways to initiate a consultation with Dr. Ravi Teja Rudraraju
You can provide current X-rays and/or MRIs for a clinical case review with with Dr. Ravi Teja Rudraraju
You can schedule an office consultation with Dr. Ravi Teja Rudraraju
Frequently Asked Questions
Osteochondritis Dissecans is an idiopathic condition affecting the subchondral bone and overlying articular cartilage, leading to segment separation, instability, pain, and joint effusion.
The exact cause is unknown but is believed to be multifactorial, involving factors like direct trauma, repetitive microtrauma, chemical changes, genetic conditions, growth disorders, hereditary factors, and ischemia.
Symptoms include vague pain, swelling, straining-dependent stabbing pain, stiffness, feelings of instability, mechanical symptoms like clicking or locking, and, in advanced cases, quadriceps muscle atrophy and gait deviations.
Diagnosis involves a combination of clinical evaluation, imaging studies like X-rays and MRI, and sometimes arthroscopy for a detailed examination of the joint.
Treatment may include conservative measures like physical therapy and activity modification, as well as surgical interventions like arthroscopy, drilling, or cartilage grafting, depending on the severity.
No, surgery is not always necessary. Mild cases may respond well to conservative treatments. However, in advanced cases or when symptoms persist, surgical intervention may be considered.
While prevention is not guaranteed, avoiding excessive repetitive stress on the knee joint, maintaining a healthy lifestyle, and addressing injuries promptly may help reduce the risk.
Recovery time varies based on the type of surgery performed. Physical therapy is typically recommended to regain strength and range of motion, and the return to normal activities depends on individual progress.
There is a possibility of recurrence, especially if predisposing factors are not addressed. Following post-treatment guidelines and regular follow-ups can help monitor the condition.
While it can affect individuals of any age, it is often seen in adolescents and young adults, particularly those involved in high-impact sports.
Conclusion:
At Dr. Ravi Teja’s clinic, we are dedicated to understanding, diagnosing, and treating Osteochondritis Dissecans of the Knee effectively. If you’re ready to take the next step towards relief, feel free to initiate a consultation through X-ray and MRI reviews or schedule an in-person visit. We look forward to guiding you on your journey to improved knee health.
Latest Post