Posterolateral Knee Injuries
Description of Posterolateral Knee Injuries
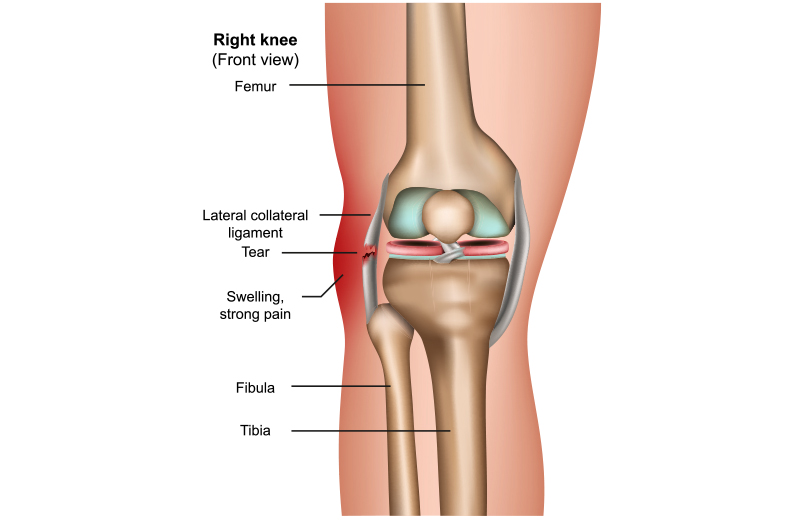
The posterolateral corner (PLC) of the knee, situated on the outside of the knee joint, plays a crucial role in stabilizing the knee against lateral or external forces, especially common in sports like football, soccer, skiing, and basketball. While PLC injuries constitute a smaller portion of knee injuries compared to ACL or MCL injuries, they can significantly impact athletic performance.
Symptoms of a PLC injury include:
Side-to-side instability
Difficulty twisting, turning and pivoting
Minimal swelling and pain along the outside of the knee
A foot drop with a concurrent peroneal nerve injury
Diagnosing and treating PLC injuries can be challenging due to the complexity of this area. Symptoms typically include side-to-side instability, difficulty with twisting and turning motions, minimal swelling and pain along the outside of the knee, and in severe cases, a foot drop due to concurrent peroneal nerve injury. Interestingly, patients may notice instability gradually over several weeks to months following the initial injury.
The main anatomical structures involved in the posterolateral aspect of the knee include the lateral collateral ligament (LCL), the popliteus tendon, the popliteofibular ligament, the lateral capsule, anterolateral ligament, and the biceps femoris attachment to the fibular head. Assessment of the common peroneal nerve is also crucial as it crosses the fibular head in close proximity to these structures, with approximately 15-20% of patients experiencing nerve injury symptoms.
Diagnosis of Posterolateral Knee Injuries
There are many tests that must be synthesized to diagnose a posterolateral corner knee injury. These include:
- Varus Stress Test – in full extension and at 30° of knee flexion
- Dial Test at 30° and 90° of knee flexion
- Posterolateral Drawer Test
- External Rotation Recurvatum Test,
Reverse Pivot Shift Test
Assessment for a Varus Thrust Gait
Diagnosis involves synthesizing various tests such as the Varus Stress Test, Dial Test, Posterolateral Drawer Test, External Rotation Recurvatum Test, Reverse Pivot Shift Test, and assessment for Varus Thrust Gait to determine the type of instability present. It’s important not to overlook a posterolateral injury, especially since about 72% of patients with PLC injuries may also have concurrent cruciate ligament injuries.
Dr. Ravi Teja Rudraraju employs a comprehensive approach, utilizing plain x-rays, stress x-rays, and MRI scans to diagnose and assess the extent of the injury. In cases where there is suspicion of concurrent PCL tears, posterior kneeling stress x-rays are also obtained to evaluate posterior translation in the injured knee. Early surgical intervention, typically within 2 to 3 weeks of the injury, is often recommended to optimize outcomes.
Posterolateral knee injuries are classified based on the severity of the injury:
Grade I Injury: This involves a small partial tear with minimal instability.
Grade II Injury: There’s a partial tear with an identifiable endpoint to stressing.
Grade III Injury: This is a complete tear with no clear endpoint to stressing.
Typically, grade III injuries are recommended for surgery due to the low likelihood of natural healing. This is primarily because of the unique anatomy of the posterolateral corner, where two opposing convex bony surfaces exist, leading to inherent bony instability.
Given the high risk of scarring and retraction of torn structures in posterolateral knee injuries, it’s generally advised that surgeries be performed within two to three weeks after the injury. This allows for early range of motion and ensures that sutures can effectively hold onto the torn structures with early post-surgery motion. This timing is crucial for optimal outcomes.
Surgical Treatment of PLC Injuries
Dr. Ravi Teja Rudraraju typically recommends a hybrid approach for repairable structures and anatomic reconstruction for midsubstance tears of the posterolateral corner in acute injuries. For chronic injuries, he generally opts for anatomic reconstructions.
Dr. Ravi Teja Rudraraju has developed multiple surgical techniques based on anatomy and biomechanical validation to address these injuries. These techniques include lateral collateral ligament reconstructions, popliteus tendon reconstructions, proximal tibiofibular joint reconstructions, and complete posterolateral corner reconstructions. All these procedures have demonstrated positive patient outcomes.
Post-Operative Care for PLC Injuries
The postoperative rehabilitation protocol involves allowing motion of 0-90 degrees for the first two weeks within the “safe zone” determined by Dr. Ravi Teja Rudraraju as he assesses stress on the repaired structures during surgery. After the initial two weeks, motion is gradually increased to full range. Patients are advised to be nonweight bearing for six weeks postoperatively and to refrain from isolated active hamstring exercises for the first four months to minimize stress on the healing posterolateral corner repair and reconstruction procedures.

Have you sustained a posterolateral knee injury?
There are two ways to initiate a consultation with Dr. Ravi Teja Rudraraju
You can provide current X-rays and/or MRIs for a clinical case review with with Dr. Ravi Teja Rudraraju
You can schedule an office consultation with Dr. Ravi Teja Rudraraju
Frequently Asked Questions
The posterolateral corner of the knee comprises structures located on the lateral and posterolateral aspects. Historically termed the “dark side” due to its complexity, our research team has extensively studied its anatomy, biomechanics, and treatment strategies. Through nearly 50 peer-reviewed articles, we’ve revolutionized its treatment with successful anatomic-based reconstruction procedures. This thorough analysis has significantly improved patient outcomes.
The posterolateral corner’s stability relies on three main static stabilizers: the fibular collateral ligament, popliteofibular ligament, and popliteus tendon. Additionally, other structures like the lateral capsule, lateral meniscus, iliotibial band, and biceps femoris contribute to stability. Injuries to these structures necessitate reconstructions to ensure optimal patient recovery.
Critical clinical tests include the varus stress test, dial test, posterolateral drawer test, and external rotation recurvatum test. These assess for various instabilities and gait abnormalities, guiding diagnosis and treatment planning.
The arcuate ligament, once termed for its curved shape, comprises several specific structures like the popliteofibular ligament and biceps femoris attachment. Recognizing its components aids in understanding knee stability and injury patterns.
Posterolateral corner injuries typically result from hyperextension, contact hyperextension, or lateral stress to the knee. Accurate diagnosis is crucial, considering the potential involvement of the common peroneal nerve in up to 15% of cases.
MRI scans help assess key structures like the fibular collateral ligament, popliteus tendon, and lateral capsule. However, diagnosing chronic fibular collateral ligament injuries can be challenging, highlighting the importance of supplementary assessments like bilateral varus stress x-rays.
Acute and chronic injuries require specific x-ray evaluations. Bilateral varus stress x-rays are particularly valuable in objectively diagnosing posterolateral corner injuries.
Compression or irritation of the common peroneal nerve often leads to posterolateral nerve pain. A thorough evaluation is necessary to differentiate between knee-related and spinal-related causes, guiding appropriate treatment.
Our surgical approach involves an incision along the iliotibial band, providing a wide view of the posterolateral knee structures. Precise measurements guide reconstructions, ensuring optimal anatomical alignment and patient outcomes.
These comprehensive approaches, combined with meticulous surgical techniques, have significantly improved the management of posterolateral corner injuries, resulting in better patient outcomes.
The FCL plays a crucial role in stabilizing the knee against lateral compartment gapping. Our team has developed an anatomic-based reconstruction technique, yielding excellent outcomes. The procedure involves harvesting a hamstring graft or using a hamstring allograft. Reconstruction tunnels are created at the FCL’s attachment sites on the femur and fibular head, with the graft secured in place using interference screws. This technique, particularly utilizing hamstring grafts, has shown remarkable success akin to ACL reconstructions.
In cases of complete tear involving the FCL, popliteus tendon, and popliteofibular ligament, a comprehensive reconstruction is warranted. Our internationally validated anatomic-based procedure involves reconstructing the three main static stabilizers. This includes placing four separate graft tunnels at specific sites in the knee to restore stability effectively. Long-term follow-up studies have confirmed the success of these reconstructions in restoring knee stability and function.
During arthroscopy, signs like the “drive-thru” sign and assessment of the lateral meniscus help diagnose posterolateral corner injuries. Viewing the lateral gutter aids in evaluating the integrity of various structures, including the popliteus tendon and lateral capsule. Additionally, bone bruising in the medial compartment may indicate a secondary sign of posterolateral corner injury, necessitating careful assessment.
Advancements in rehabilitation emphasize early range of motion to prevent stiffness and improve patient function. Our protocols advocate for early motion postoperatively, coupled with partial weight-bearing to aid in patient recovery. These protocols have shown promising results in enhancing patient outcomes and minimizing complications.
Latest Post